This page is for general education only and does not replace medical care. If you have severe chest pain, trouble breathing, confusion, or sudden weakness, seek urgent medical help.
Lupus overview: what SLE is and why symptoms vary
Definition
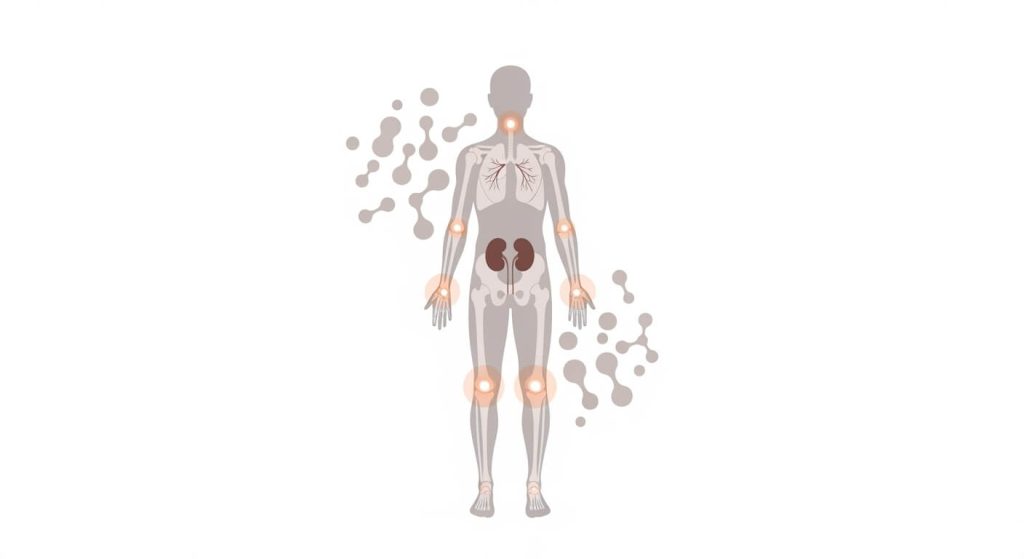
Lupus is an autoimmune condition where the immune system mistakenly attacks healthy tissues, leading to inflammation that can involve multiple organs and systems—commonly joints and skin, and sometimes kidneys, lungs, heart, blood vessels, and the nervous system.
Lupus can be challenging to recognize because symptoms can overlap with other conditions and may come and go in “flares,” with quieter periods in between.
Why lupus happens: triggers and risk patterns
Causes
The exact cause of lupus isn’t fully known. Most explanations involve a mix of genetic susceptibility plus environmental factors that can help trigger immune overactivity in someone who is predisposed.
Common triggers (examples)
- Sun or UV exposure (can worsen skin symptoms in some people)
- Infections (may precede or worsen flares for some people)
- Certain medications (some cases are medication-triggered and may improve after stopping the trigger under clinician guidance)
Risk factors (patterns seen in populations)
- Sex assigned female at birth (diagnosed more often in this group)
- Age (often diagnosed in teen years through mid-adulthood, though it can occur at any age)
- Race/ethnicity patterns (higher observed rates in some populations, including Black, Hispanic, and Asian American groups in the U.S.)
Common symptoms and flare patterns
Symptoms
Symptoms can differ widely based on which body systems are involved and whether the condition is in a flare. Common symptoms include:
- Ongoing fatigue and/or fever
- Joint pain, stiffness, and swelling
- Skin rashes, including a “butterfly-shaped” rash across the cheeks and nose in some people
- Sun sensitivity (rashes can worsen with sunlight for some people)
- Fingers or toes that change color with cold or stress (Raynaud-type changes can be harder to see on darker skin tones)
- Shortness of breath or chest pain (possible lung/heart involvement—needs evaluation)
- Headaches, confusion, or memory issues (possible nervous system involvement—needs evaluation)
When to seek medical care
Seek evaluation if you develop persistent symptoms (rash, joint swelling, unexplained fevers, chest pain, shortness of breath, neurologic symptoms, or swelling/foamy urine). Seek urgent care for severe chest pain, trouble breathing, fainting, new confusion, or sudden weakness.
How lupus is diagnosed
Diagnosis
Diagnosis is clinical (symptoms + exam) and typically supported by labs. A common blood test used during evaluation is an ANA (antinuclear antibody) test, which can help clinicians assess whether an autoimmune condition like systemic lupus erythematosus may be present (results must be interpreted in context).
Depending on symptoms, clinicians may also use:
- Blood counts to look for anemia or other blood-cell changes
- Urine and kidney function testing (kidney involvement is an important concern)
- Additional antibody and inflammation testing (selected based on the case)
- Imaging or specialist evaluation if organs like lungs, heart, or brain may be involved
- Sometimes, a tissue biopsy (for example, when kidney disease is suspected and confirmation matters for treatment planning)
Medications used to manage lupus
Medications
Medication choices depend on which organs are involved, how active symptoms are, and a person’s overall risk profile. Plans are always individualized by a licensed clinician.
Common medication “buckets” include:
- Symptom-relief options (used selectively for pain/inflammation)
- Steroids (often used for flares or organ-threatening inflammation, then tapered when possible)
- Immune-modifying therapies (to reduce immune-driven inflammation)
- Targeted biologic therapies in selected cases
If you already have a clinician-guided plan and valid prescriptions and you’re exploring affordability options, a safety-first framework matters—start with the Certified Medical Tourism Professional guide and review pharmacy evaluation basics in Pharmacies in Tijuana (2025).
Treatment and long-term management
Treatments
Lupus care usually combines medical treatment plus practical long-term management to reduce flares and protect organs.
Common care elements include:
- Regular monitoring (symptoms, labs, and organ function—especially kidneys and blood counts)
- Trigger awareness (for example, UV exposure) and individualized prevention strategies
- Managing cardiovascular risk over time when relevant (because inflammation can affect long-term health)
- Coordinated care for pregnancy planning (important because pregnancy can carry higher risks in lupus and timing matters)
- Mental health support when needed (chronic illness can be emotionally heavy, especially during flares)
People also ask about lupus
FAQs
What are the first signs of lupus?
Early signs vary, but common early patterns include fatigue, fevers, joint pain/swelling, and skin rashes—sometimes with sun sensitivity. Because these symptoms overlap with many other conditions, evaluation is important.
Can lupus be hard to diagnose?
Yes. Lupus can look like other illnesses and symptoms may come and go. Clinicians typically use symptom history, exam findings, and supportive lab testing to make the diagnosis.
Is the “butterfly rash” required to have lupus?
No. Some people develop a butterfly-shaped facial rash, but many do not. Lupus can affect different body systems, so skin findings are only one possible part of the picture.
What triggers lupus flares?
Triggers differ by person, but sunlight/UV exposure, infections, and certain medications are commonly discussed triggers in people who are predisposed.
What complications can lupus cause?
Complications depend on which organs are involved. Kidney disease is a major concern, and lupus can also affect the brain/nervous system, blood and blood vessels (including clotting issues), lungs, and heart.


