Rheumatoid arthritis overview
Rheumatoid arthritis is a long-term (chronic) condition that causes joint pain, swelling, and irritation (inflammation). While it often starts in the joints, it can also affect other areas of the body over time, including the skin, eyes, lungs, heart, and blood vessels.
This condition happens when the immune system mistakenly attacks healthy tissues. Because it is autoimmune, symptoms may come and go—many people with rheumatoid arthritis experience “flares” (when symptoms worsen) and periods of improvement (remission). With modern care, many patients can manage symptoms and protect joint function, especially when rheumatoid arthritis is recognized early.
Definition
What is rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune disease that typically targets the lining of the joints (the synovium). Over time, persistent inflammation can damage cartilage and bone and may change the shape of a joint, which is why early evaluation matters.
It is different from osteoarthritis. Osteoarthritis is often associated with wear-and-tear and mechanical joint breakdown, while autoimmune arthritis is driven by inflammation and immune activity. Some people can have features of more than one joint condition, so diagnosis should be confirmed by a licensed clinician.
Causes
There is no single known cause. Experts believe rheumatoid arthritis develops from a combination of:
- Genetic susceptibility (family history can increase risk)
- Environmental factors (certain exposures may trigger immune changes)
- Hormonal influences (patterns differ by sex)
In some people, infections may contribute to immune activation, but infection is not considered the typical direct cause of this chronic condition.
Symptoms
In rheumatoid arthritis, symptoms can vary in severity and may develop gradually. Common symptoms include:
- Painful, warm, swollen joints
- Stiffness that is often worse in the morning or after rest (sometimes lasting 45–60+ minutes)
- Fatigue, low fever, and reduced appetite
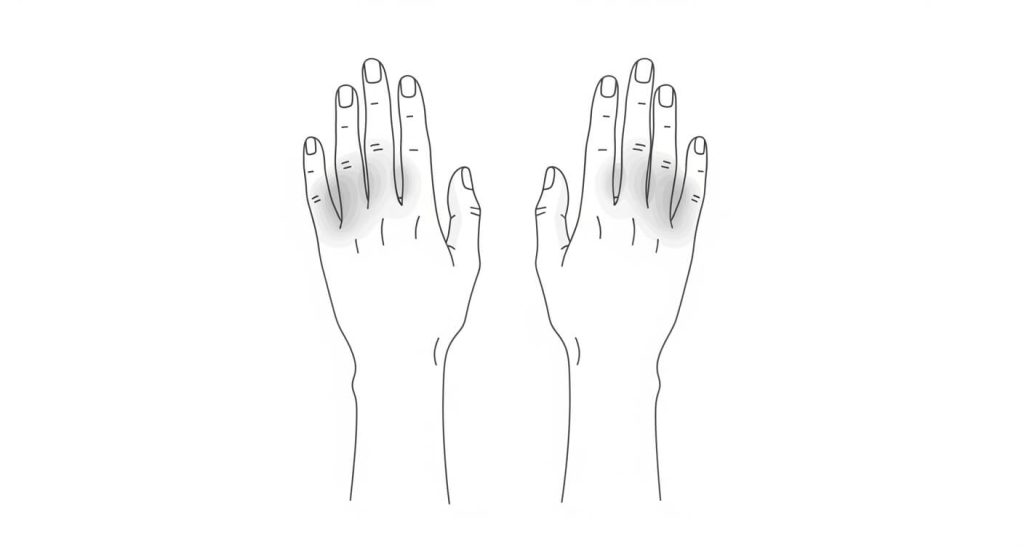
- Symptoms beginning in smaller joints (hands and feet) and potentially spreading to wrists, elbows, hips, knees, and ankles
- Symptoms often affecting the same joints on both sides of the body
Because inflammation can be systemic, rheumatoid arthritis may also cause symptoms beyond the joints. That can include eye irritation, skin changes, shortness of breath, or unusual chest discomfort—signs that warrant medical attention.
When to see a doctor
Make an appointment with a healthcare professional if you have joint pain and swelling that doesn’t improve after several weeks—especially if morning stiffness persists, symptoms are symmetric (both sides), or daily activities are becoming harder.
If you suspect rheumatoid arthritis may be behind ongoing joint symptoms, getting evaluated sooner can help protect joint function and guide next steps.
Seek urgent evaluation if you have severe shortness of breath, chest pain, sudden weakness, or symptoms that feel rapidly worsening.
Diagnosis
Rheumatoid arthritis is diagnosed by a licensed clinician using symptoms, a physical exam, and testing to confirm inflammation and rule out other causes of joint pain.
Diagnosis often involves:
- A clinical history focused on symptom pattern (morning stiffness, symmetric joints, flares/remission)
- Joint exam for swelling, warmth, tenderness, and range of motion
- Blood tests to assess inflammation and immune markers (as appropriate)
- Imaging (such as X-ray or ultrasound) to evaluate joint changes or inflammation
Because several conditions can mimic rheumatoid arthritis, testing and interpretation should be done by a licensed medical team.
Medications
Medication choices are individualized and must be guided by a licensed clinician. Management may include:
- Anti-inflammatory or pain-relieving medications (as appropriate)
- Disease-modifying therapies prescribed and monitored by clinicians
Never start, stop, or change medications without medical guidance.
Treatments
Treatment and long-term management
Treatment for rheumatoid arthritis is individualized and guided by a licensed clinician (often a rheumatologist). The goal is to reduce inflammation, control symptoms, prevent joint damage, and protect quality of life.
Management plans often include:
- Anti-inflammatory or pain-relieving medications (as appropriate)
- Disease-modifying therapies prescribed and monitored by clinicians
- Physical therapy or guided exercise to maintain mobility and strength
- Occupational therapy strategies to protect joints during daily activities
- Lifestyle changes such as quitting tobacco, maintaining a healthy weight, and protecting sleep
Regular follow-up matters because treatment needs can change over time. Many people do best with a plan that addresses both flare control and long-term prevention of joint damage in rheumatoid arthritis.
FAQs
Is rheumatoid arthritis the same as osteoarthritis?
No. Osteoarthritis is often associated with wear-and-tear and mechanical joint breakdown. Rheumatoid arthritis is autoimmune and driven by inflammation and immune activity.
Why does morning stiffness matter?
Morning stiffness that lasts 45–60+ minutes (or longer) can be a clue that inflammation is involved, which is one reason clinicians evaluate for autoimmune arthritis.
Can rheumatoid arthritis affect more than joints?
Yes. Rheumatoid arthritis can be systemic and may affect the skin, eyes, lungs, heart, and blood vessels over time. New shortness of breath, chest discomfort, or eye symptoms should be discussed with a clinician.
What are “flares” and “remission”?
A flare is a period when symptoms worsen and inflammation increases. Remission is a period when symptoms improve significantly or are minimal.
What should I do if I think I have rheumatoid arthritis?
Schedule an evaluation with a licensed clinician—especially if joint swelling, symmetric symptoms, or morning stiffness are persistent. Early evaluation can help protect joint function.


