Ulcerative Colitis Overview
Definition
Ulcerative colitis is a form of inflammatory bowel disease (IBD) in which the immune system triggers ongoing inflammation and ulceration on the inner lining of the large intestine (colon) and rectum.
Symptoms often build gradually over time and the condition can range from mild to severe. With the right medical care, many people can reduce symptoms and achieve periods of remission.
Educational note: This page is for general information only and does not replace medical advice. If you’re experiencing new or worsening symptoms, contact a licensed clinician.
What is ulcerative colitis?
Ulcerative colitis is a chronic condition where inflammation typically begins in the rectum and may extend upward through part or all of the colon. Unlike Crohn’s disease (which can involve any part of the digestive tract and deeper layers of the bowel wall), ulcerative colitis is limited to the colon and rectum and primarily affects the innermost lining.
Even though there isn’t a single “one-size-fits-all” cure, modern treatment plans can be very effective at controlling inflammation, easing symptoms, and helping protect the colon over the long term.
Types
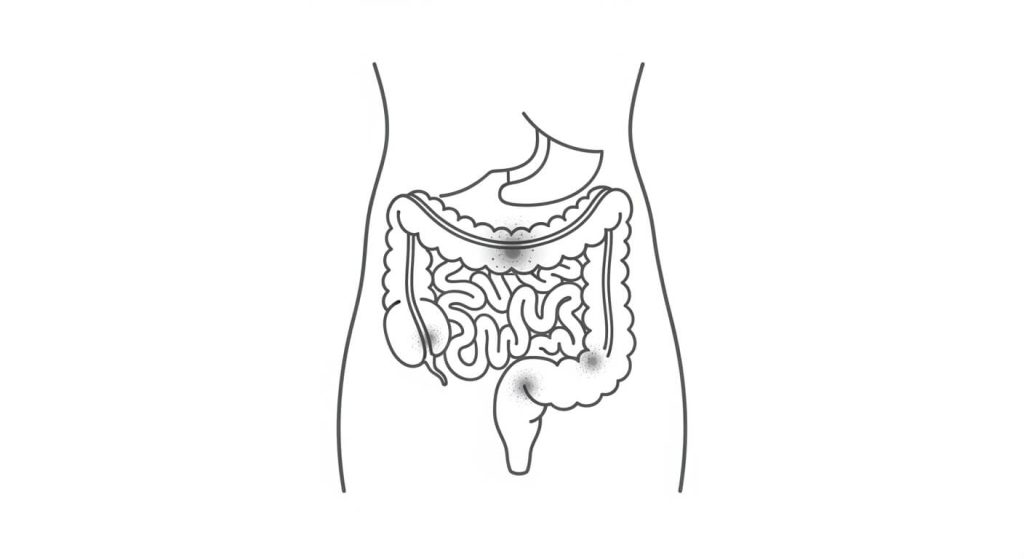
Clinicians often describe ulcerative colitis by where it’s located in the large intestine:
Ulcerative proctitis
Inflammation is limited to the rectum. Symptoms may include rectal bleeding, urgency, and rectal discomfort.
Left-sided colitis
Inflammation extends from the rectum into the sigmoid and/or descending colon. Some people experience cramping, bloody diarrhea, and the sensation of needing to go even when the bowel is empty (tenesmus).
Extensive colitis (pancolitis)
Inflammation affects most or all of the colon and may be associated with more intense symptoms such as frequent bloody diarrhea, fatigue, and weight loss.
Related conditions: Crohn’s disease and microscopic colitis can also cause intestinal inflammation and diarrhea, but they differ in location, depth of involvement, and diagnostic findings.
Ulcerative Colitis Symptoms and When to Seek Care
Symptoms
Symptoms vary by person and by how active the inflammation is. Common symptoms include:
- Diarrhea (often urgent), sometimes with blood, mucus, or pus
- Rectal bleeding or blood in the stool
- Abdominal cramping or pain
- Rectal pain or pressure
- Tenesmus (feeling like you need to pass stool even when you can’t)
- Fatigue
- Fever (more common in moderate/severe flares)
- Weight loss
- In children, slowed growth or delayed development
Many people experience flares and remissions—periods where symptoms calm down significantly.
When to see a doctor
Consider medical evaluation if you notice bowel changes that persist, or symptoms such as:
- Blood in your stool
- Persistent or worsening diarrhea
- Abdominal pain that doesn’t improve
- Fever lasting more than 1–2 days, especially with dehydration
- Symptoms that wake you from sleep
Seek urgent care immediately for severe dehydration, heavy rectal bleeding, fainting, or intense abdominal pain.
What Causes Ulcerative Colitis?
Causes
The exact cause isn’t fully known. Research suggests ulcerative colitis involves a combination of:
- Immune dysregulation (the immune system reacts abnormally and fuels inflammation)
- Genetics (higher risk if close family members are affected)
- Microbiome factors (imbalances in gut bacteria may contribute)
- Environmental influences (factors like geography, certain exposures, and antibiotic use are being studied)
Diet and stress are not considered the root cause, but they can worsen symptoms during flares for some people.
Risk factors
Ulcerative colitis can affect anyone, but common risk patterns include:
- Family history of IBD
- Age (often diagnosed before 30, though it can appear later)
- Certain ancestry/ethnic backgrounds may have higher observed rates in some populations
How Ulcerative Colitis Is Diagnosed
Diagnosis
Ulcerative colitis is diagnosed by combining your symptom history, a physical exam, and tests that help confirm inflammation in the colon and rule out other causes.
Common parts of the diagnostic process
- Medical history and exam: A clinician reviews bowel changes, bleeding, abdominal pain, fever, weight loss, and family history of IBD, and checks for signs of dehydration or anemia.
- Lab tests: Blood work may be used to look for anemia or signs of inflammation, and stool tests can help rule out infections that may mimic ulcerative colitis.
- Endoscopy: A colonoscopy (or sigmoidoscopy) allows a specialist to directly view the colon lining and assess where inflammation is located.
- Biopsy: Small tissue samples taken during endoscopy can help confirm ulcerative colitis and exclude other conditions.
- Imaging (when needed): In some cases, imaging is used to evaluate complications or help clarify the extent of disease.
Because ulcerative colitis can look similar to other digestive conditions, diagnosis depends on confirming the pattern and location of inflammation and excluding infections and other causes.
Ulcerative Colitis Medicines and Biologic Therapy
Medications
A note on treatment and medication access
Treatment is individualized and may include anti-inflammatory medicines, immune-modifying therapies, and biologics—your gastroenterologist will guide what’s appropriate for your case.
If you’ve been prescribed a high-cost therapy, you may also want to read our guide on Stelara assistance options (often discussed for IBD medication affordability).
Ulcerative Colitis Treatment Planning and Safety Considerations
Treatments
And if you’re exploring cross-border options for prescriptions, our overview of pharmacies in Tijuana explains what people typically look for when evaluating pharmacies and safety considerations.
Complications
Ulcerative colitis can cause serious complications—especially if inflammation is uncontrolled. Examples include:
- Severe bleeding and anemia
- Dehydration
- Bone loss (osteoporosis)
- Inflammation outside the gut (skin, joints, eyes)
- Increased risk of colon cancer (risk varies by duration and extent of disease)
- Toxic megacolon (rare but life-threatening enlargement of the colon)
- Increased risk of blood clots
- Growth delay in children
Ulcerative Colitis FAQs
FAQs
How do I know if my symptoms could be ulcerative colitis?
Ulcerative colitis symptoms often build gradually and can vary from mild to severe. Common patterns include ongoing diarrhea (often urgent) that may contain blood, mucus, or pus, along with rectal bleeding, abdominal cramping, rectal pain or pressure, and fatigue. Many people experience flares and remissions—periods where symptoms calm down significantly.
What should I do if I notice blood in my stool or persistent diarrhea?
Consider medical evaluation if you notice bowel changes that persist, including blood in your stool, persistent or worsening diarrhea, or abdominal pain that doesn’t improve. If symptoms are new or worsening, contact a licensed clinician so the cause can be assessed and the right next steps can be determined.
When is ulcerative colitis an emergency?
Seek urgent care immediately for severe dehydration, heavy rectal bleeding, fainting, or intense abdominal pain. Also consider urgent evaluation if you have a fever lasting more than 1–2 days, especially with dehydration, or symptoms that wake you from sleep.
Why do symptoms come and go?
Many people with ulcerative colitis experience cycles of flares and remissions. Symptoms can worsen when inflammation is more active and improve when inflammation is better controlled. While diet and stress are not considered the root cause, they can worsen symptoms during flares for some people.
Can ulcerative colitis cause long-term complications if it isn’t controlled?
Yes. Ulcerative colitis can cause serious complications—especially if inflammation is uncontrolled. Examples include severe bleeding and anemia, dehydration, bone loss (osteoporosis), inflammation outside the gut (skin, joints, eyes), increased risk of colon cancer (risk varies by duration and extent of disease), toxic megacolon (rare but life-threatening enlargement of the colon), increased risk of blood clots, and growth delay in children.
A note on treatment and medication access
Treatment is individualized and may include anti-inflammatory medicines, immune-modifying therapies, and biologics—your gastroenterologist will guide what’s appropriate for your case.
If you’ve been prescribed a high-cost therapy, you may also want to read our guide on Stelara assistance options (often discussed for IBD medication affordability).
And if you’re exploring cross-border options for prescriptions, our overview of pharmacies in Tijuana explains what people typically look for when evaluating pharmacies and safety considerations.
For a deeper medical overview of ulcerative colitis (definition, symptoms, causes), see the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Ulcerative Colitis (NIDDK).


