Educational note: This content is for education only and does not replace medical advice. If you have persistent fever, severe weakness, uncontrolled bleeding, new confusion, or rapidly worsening shortness of breath, seek urgent medical evaluation.
Definition
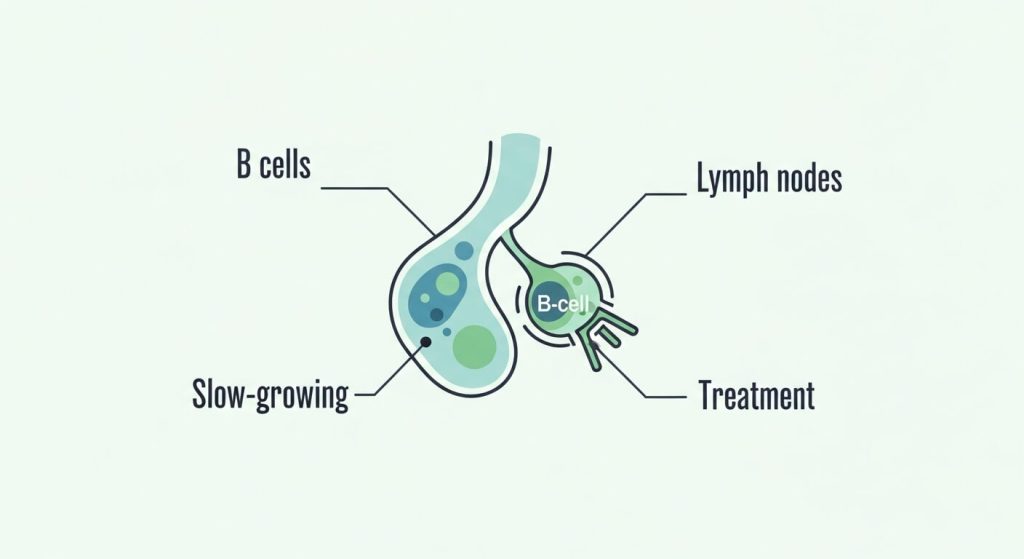
What Follicular Lymphoma is: a slow-growing B-cell non-Hodgkin lymphoma
Follicular Lymphoma is a type of non-Hodgkin lymphoma that begins in B cells (white blood cells that help your immune system). It often starts inside lymph node “follicles,” where B cells normally mature and respond to infections. In Follicular Lymphoma, abnormal B cells multiply and can collect in lymph nodes, bone marrow, and other lymphatic tissues.
Many cases behave in an indolent (slow-growing) way. That slower pace can change how doctors approach care, including whether treatment needs to start right away or whether careful monitoring is appropriate.
Why the lymphatic system matters
The lymphatic system helps move immune cells, filter fluid, and support infection-fighting. When lymphoma involves this system, it can affect:
- Lymph nodes (neck, armpit, groin, chest, abdomen)
- Spleen
- Bone marrow
- Less commonly, other organs
A key concept: “transformation”
In some people, Follicular Lymphoma can transform into a faster-growing lymphoma. This is one reason follow-up plans and symptom tracking matter—even if the disease is slow at the start.
Causes
Why this lymphoma happens: immune-cell changes and risk patterns
The exact cause isn’t always identifiable. Most often, Follicular Lymphoma develops after genetic changes build up in B cells over time. These changes can affect how cells grow, survive, and respond to immune signals.
Rather than one clear trigger, clinicians typically talk about risk factors—things associated with higher likelihood, but not direct causes for most individuals.
Risk factors linked to higher risk
- Older age (more common later in adulthood)
- Family history of lymphoma (in some cases)
- Immune suppression (depending on the situation)
- Certain autoimmune or immune-related conditions (varies by person)
Important reassurance
Many people diagnosed with Follicular Lymphoma have no obvious exposure or preventable cause. It can happen even when someone has lived a healthy lifestyle.
Symptoms
Symptoms to watch: swollen nodes, “B symptoms,” and subtle clues
Follicular Lymphoma may cause no symptoms for a long time. Some people find out after an exam or imaging for another reason. When symptoms do appear, they often relate to lymph node enlargement or broader immune effects.
Common symptoms
- Painless swelling of lymph nodes (neck, armpit, groin)
- Persistent fatigue
- Fever without a clear infection
- Night sweats (especially drenching)
- Unintentional weight loss
- Feeling full quickly or abdominal discomfort (possible spleen or abdominal node enlargement)
Symptoms that can suggest low blood counts (when marrow is involved)
- Shortness of breath with mild activity
- Dizziness or paleness
- Increased bruising or bleeding (less common, but possible)
When to call urgently
Seek urgent care for:
- Fever with severe weakness or dehydration
- Rapidly worsening shortness of breath or chest pain
- Significant bleeding, black stools, or vomiting blood
- New confusion, fainting, or severe headache
Diagnosis
How Follicular Lymphoma is diagnosed: biopsy, imaging, and staging
Diagnosis is usually step-by-step: confirm lymphoma, identify the subtype, and determine how widespread it is. Because different lymphomas can look similar early on, tissue diagnosis is often essential.
Core tests used in diagnosis
- Physical exam (lymph nodes, spleen)
- Blood tests (blood counts and organ function)
- Imaging (CT and/or PET/CT to map involved areas)
- Lymph node biopsy (often required to confirm the subtype)
- Bone marrow evaluation (sometimes needed)
Why biopsy is so important
A biopsy helps your team:
- Confirm Follicular Lymphoma vs. other subtypes
- Assess grade and biologic behavior
- Identify markers that can guide therapy choices
For a clinician-reviewed overview of typical workup and treatment approaches, see Mayo Clinic’s Follicular lymphoma diagnosis and treatment.
Helpful questions after diagnosis
- What subtype and grade do I have?
- Is this low-burden disease or high tumor burden?
- Do I need treatment now, or is observation reasonable?
- What symptoms should trigger a call right away?
Medications
Medicines used in Follicular Lymphoma: immune therapy, targeted drugs, and supportive care
Medication choices depend on symptoms, tumor burden, stage, grade, and overall health. Some people start therapy immediately; others begin later if the disease becomes more active.
Medication categories commonly used
- Monoclonal antibodies that target B cells
- Chemo-immunotherapy combinations (chemotherapy + antibody)
- Targeted therapy aimed at pathways lymphoma cells rely on
- Steroids in specific regimens or for symptom control
- Supportive medications to reduce side effects and complications
Supportive medications are part of treatment
Supportive care can include:
- Anti-nausea medications
- Infection-prevention strategies in selected cases
- Medications for pain, sleep, or appetite when clinically appropriate
If drug names or pricing differences feel confusing during planning, this explainer can help: Generic vs. brand-name drugs: what changes and what doesn’t.
Treatments
Treatment options for Follicular Lymphoma: observation, radiation, systemic therapy, and advanced care
Care is personalized. The goal is to match treatment intensity to the way the disease is behaving—avoiding overtreatment when it’s slow and acting promptly when it becomes more active.
Watchful waiting (active surveillance)
For low-burden Follicular Lymphoma without symptoms or organ risk, “watch and wait” may be recommended. This involves scheduled follow-ups, labs, and imaging when needed. It’s not ignoring the disease—it’s choosing the right timing.
Radiation therapy (when localized or for symptom relief)
Radiation may be used when disease is limited to one area or when a specific site causes symptoms, discomfort, or compression.
Systemic therapy (when widespread or symptomatic)
When treatment is needed, options may include:
- Immunotherapy-based regimens
- Combination regimens that include chemotherapy
- Targeted therapies based on clinical factors
- Clinical trials (especially for relapse or higher-risk disease)
Advanced options for relapsed or resistant disease
In selected situations, specialized therapies (including cell-based approaches) may be considered in experienced centers, particularly after multiple prior therapies.
If you’re coordinating care between locations, gathering records, or planning a second opinion, this resource can help you stay organized: Certified medical tourism professional guide.
FAQs
Follicular Lymphoma FAQs: practical answers in plain language
Can Follicular Lymphoma be cured?
Some people achieve long remissions and do very well for many years. Whether it’s “curable” depends on factors like grade, extent of disease, and response to therapy. Your specialist can frame expectations for your specific case.
Why would a doctor recommend watchful waiting?
Because this lymphoma can grow slowly, immediate treatment may not improve outcomes for everyone—especially if there are no symptoms, organ risks, or high tumor burden. Monitoring can be the safest option until treatment is clearly beneficial.
What symptoms should make me contact my care team quickly?
Persistent fevers, rapidly enlarging lymph nodes, drenching night sweats, unintentional weight loss, new abdominal fullness/pain, or a noticeable change in energy level should prompt a call—especially if symptoms are new or escalating.
Can it turn into a faster-growing lymphoma?
Yes. Follicular Lymphoma can transform into a more aggressive type in some people. A sudden change in symptoms (rapid node growth, worsening fevers, or sharp decline in how you feel) should be evaluated promptly.
What tests guide treatment decisions the most?
A biopsy confirms subtype and key features like grade. Imaging helps map extent of disease, and blood tests help assess organ function and overall safety for different treatment options.
References
References for Follicular Lymphoma: trusted information sources
Because therapies evolve, rely on clinician-reviewed resources and your hematology/oncology team for the most current guidance. The Mayo Clinic resource linked above is a practical starting point, and your specialist can tailor recommendations to your subtype, goals, and overall health.


