Inflammatory bowel disease is an umbrella term for conditions that cause ongoing swelling and inflammation in the digestive tract. The two most common forms are Crohn’s disease and ulcerative colitis. Symptoms often include abdominal pain, diarrhea, rectal bleeding, fatigue, and unintended weight loss.
Educational note: This page is for general information only and does not replace medical advice. If you have severe pain, heavy bleeding, fainting, confusion, or signs of dehydration, seek urgent medical care.
Inflammatory Bowel Disease Overview
Definition
Inflammatory bowel disease (often shortened to IBD) refers to chronic conditions where the immune system contributes to inflammation in the digestive tract.
Crohn’s disease vs. ulcerative colitis
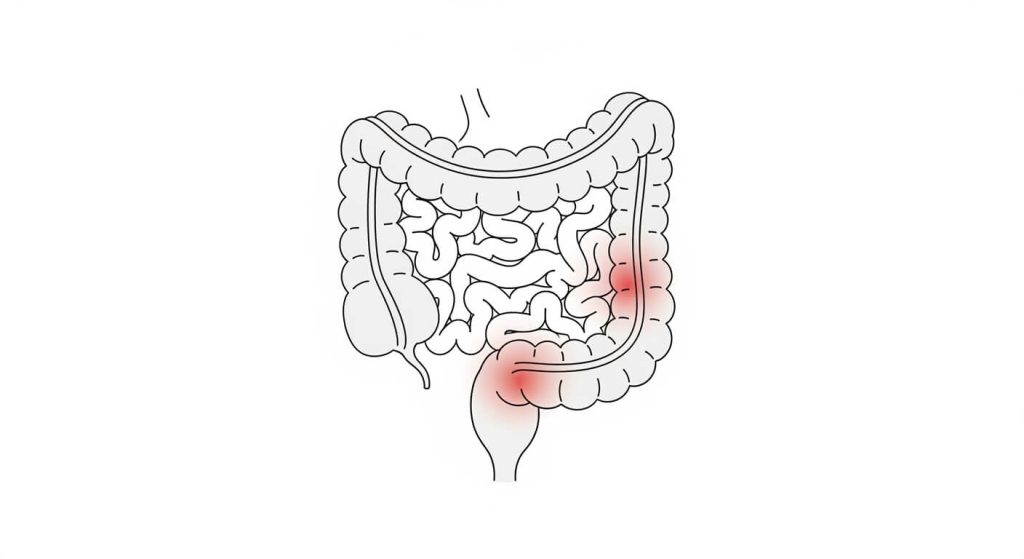
- Ulcerative colitis typically causes inflammation and ulcers along the inner lining of the colon and rectum.
- Crohn’s disease can involve inflammation anywhere in the digestive tract and may affect deeper layers of the bowel wall. It most often involves the small intestine, but it can also affect the colon and sometimes the upper GI tract.
What to expect over time
Inflammatory bowel disease usually follows a pattern of flares (active symptoms) and remission (symptoms calm down). For some people it stays mild; for others it can lead to serious complications and disability without consistent medical care.
Causes and Risk Factors for Inflammatory Bowel Disease
Causes
The exact cause of inflammatory bowel disease is not fully known. Current evidence suggests it develops from a combination of factors rather than a single trigger.
Immune system changes
One common theory is that an unusual immune response—sometimes after exposure to a virus or bacteria—causes the immune system to mistakenly attack cells in the digestive tract.
Genetics
Certain genetic markers are linked to higher risk. Inflammatory bowel disease is more common in people with close family members who have it, though many people diagnosed do not have a family history.
Environmental and microbiome triggers
Researchers also study how environment and the gut microbiome may influence risk. Factors associated with higher risk patterns in some studies include:
- Limited early-life exposure to germs (very “sterile” environments)
- A gastrointestinal infection early in life
- Antibiotic use during the first year of life
- Mostly bottle-feeding in infancy
Important clarification about diet and stress
Diet and stress are not considered the root cause of inflammatory bowel disease, but they can worsen symptoms for some people during flares.
Symptoms and When to Seek Care
Symptoms
Inflammatory bowel disease symptoms depend on how severe the inflammation is and where it occurs. Symptoms can range from mild to severe and may come and go.
Common symptoms (Crohn’s disease and ulcerative colitis)
- Diarrhea
- Abdominal pain and cramping
- Blood in the stool (or rectal bleeding)
- Reduced appetite
- Unintended weight loss
- Feeling extremely tired (fatigue)
When to seek medical evaluation
See a licensed clinician if you have a lasting change in bowel habits or persistent symptoms that concern you. While inflammatory bowel disease is often manageable, it can lead to serious complications in some people.
Seek urgent care right away if you have
- Heavy rectal bleeding or black/tarry stools
- Severe abdominal pain with repeated vomiting
- Signs of dehydration (fainting, confusion, very little urine, severe weakness)
- High fever with worsening GI symptoms
How Inflammatory Bowel Disease Is Diagnosed
Diagnosis
Diagnosing inflammatory bowel disease usually involves confirming inflammation, ruling out infections or other causes, and determining whether the pattern fits Crohn’s disease or ulcerative colitis.
Typical evaluation steps
- Medical history and exam: symptom pattern, weight changes, family history, and flare triggers
- Blood tests: anemia, inflammation markers, nutrition status
- Stool tests: check for infection and inflammation markers; evaluate blood or mucus
- Colonoscopy with biopsy: often the most direct way to assess inflammation and confirm diagnosis
- Imaging (as needed): CT or MRI-based studies can help evaluate parts of the bowel not easily seen on scope, especially when Crohn’s disease is suspected
Why “location” matters
Because inflammatory bowel disease can affect different areas and layers of the digestive tract, clinicians use test results to map where inflammation is happening and how extensive it is—this helps guide treatment.
Medications Used for Inflammatory Bowel Disease
Medications
Medication choices depend on whether you have Crohn’s disease or ulcerative colitis, how severe the inflammation is, and whether complications are present. Your clinician will tailor therapy to your disease pattern and risk level.
Common medication categories
- Anti-inflammatory medications (often used for certain ulcerative colitis patterns)
- Corticosteroids (often short-term for flares; not ideal as a long-term plan)
- Immune-modifying medications (to reduce immune-driven inflammation)
- Biologic therapies (target specific inflammation pathways; often used for moderate/severe disease)
- Antibiotics (selected situations, such as certain complications)
- Supportive medications (diarrhea control, pain support, iron/vitamins when needed—only with clinician guidance)
Important: Do not start, stop, or combine IBD medications without a licensed clinician, because safety and monitoring are a big part of effective care.
Treatment Strategies and Long-Term Care
Treatments
Treatment for inflammatory bowel disease usually combines medication, monitoring, and lifestyle support. The goals are to reduce inflammation, relieve symptoms, prevent complications, and protect quality of life.
Core treatment strategies
- Treat-to-target medical care: adjusting therapy until inflammation is controlled (not just symptoms)
- Nutrition and hydration support: especially during flares or weight loss
- Monitoring and prevention: vaccinations, bone health, and infection prevention depending on medications
- Cancer surveillance: long-standing colitis that involves much of the colon can raise colon cancer risk; clinicians may recommend scheduled colonoscopies
- Surgery (when needed): may be required for complications like strictures, fistulas, severe disease, or cancer risk management (especially in certain ulcerative colitis cases)
Practical note for prescriptions and affordability
If you already have a clinician-guided plan and valid prescriptions, some people explore cost-saving options with a safety-first process. Start with our Certified Medical Tourism Professional guide and review pharmacy verification basics in Pharmacies in Tijuana (2025).
Frequently Asked Questions About IBD
FAQs
Is inflammatory bowel disease the same as IBS?
No. Inflammatory bowel disease involves measurable inflammation and tissue injury. IBS (irritable bowel syndrome) causes symptoms like abdominal pain and bowel changes but does not cause the same type of chronic intestinal inflammation.
Can inflammatory bowel disease be cured?
There isn’t a single guaranteed cure for inflammatory bowel disease, but many people achieve long periods of remission with modern treatment plans and monitoring.
How do I know if my symptoms could be IBD?
Persistent diarrhea, abdominal pain, blood in stool, weight loss, and severe fatigue are common warning signs. Because many conditions can mimic these symptoms, testing (especially stool tests and colonoscopy) is important.
What foods should I avoid if I have IBD?
Triggers vary by person. During flares, some people tolerate low-fiber or bland diets better, while others need different adjustments. It’s best to work with a licensed clinician and/or dietitian so changes support nutrition rather than restrict it unnecessarily.
When is surgery considered?
Surgery may be recommended if medications don’t control inflammation, if complications occur (like strictures, fistulas, or severe bleeding), or when cancer risk management becomes part of care—depending on the specific IBD type and severity.


