Prostate cancer overview
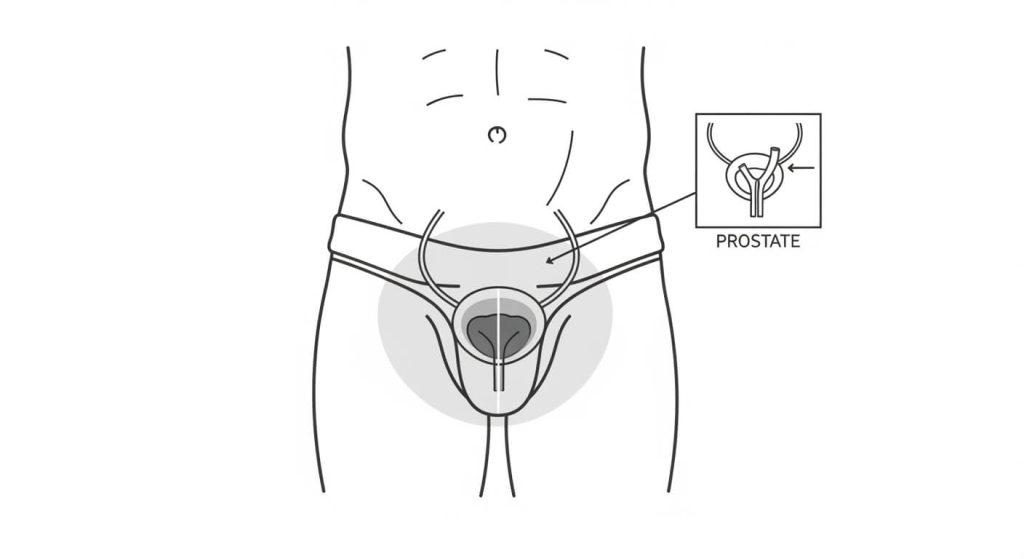
Prostate cancer is a growth of cells that begins in the prostate, a small gland located just below the bladder that helps make semen. Many cases are found early, and some tumors grow slowly—so people often have time to review options with a qualified clinician and choose the approach that fits their situation.
This page is for education only and does not replace medical advice. If you have severe pain, sudden weakness/numbness, confusion, or you cannot urinate, seek urgent medical care.
Definition
What is prostate cancer?
Prostate cancer starts when prostate cells develop DNA changes (mutations) that affect how they grow and survive. Over time, abnormal cells can build up and form a tumor. Some tumors remain localized to the prostate, while others can spread to nearby lymph nodes or distant sites like bone (metastatic disease).
A key challenge is that early prostate cancer usually causes no symptoms, which is why it’s often detected during screening discussions or evaluations done for other reasons.
Causes
For many people, the exact cause isn’t known. What’s understood is that prostate cancer begins when DNA changes in prostate cells alter normal growth signals, allowing abnormal cells to multiply and survive longer than they should—eventually forming a tumor.
Symptoms
Many people won’t notice symptoms at first. When symptoms do occur, they may include urinary changes such as a weak stream, difficulty starting urination, urinating more often (including at night), or blood in the urine or semen.
If prostate cancer becomes advanced, symptoms may relate to spread—commonly bone pain (often in the back, hips, or ribs), fatigue, unintended weight loss, and sometimes weakness or numbness in the legs or feet.
Important: urinary symptoms can also come from non-cancer causes like benign prostate enlargement or prostatitis, so it’s best to get evaluated instead of self-diagnosing.
When to see a doctor
Make an appointment if you have persistent urinary changes, blood in urine/semen, pelvic discomfort, new erectile issues, or unexplained weight loss or fatigue. Seek urgent care for severe back pain with leg weakness/numbness, or rapidly worsening symptoms.
If you’re considering screening, CDC recommends that men ages 55–69 make an individual decision after discussing benefits and harms with a clinician, and notes that men 70+ should not be routinely screened.
Diagnosis
How prostate cancer is diagnosed
Screening and diagnosis discussions often involve a PSA blood test and sometimes a digital rectal exam (DRE). If results are abnormal, a clinician may recommend additional testing (such as imaging) and/or a biopsy to confirm whether cancer is present and to understand how aggressive it looks.
Because PSA can be influenced by multiple factors, interpretation is best done with a clinician who can weigh symptoms, risk factors, and next-step options.
Medications
Medication choices depend on cancer stage, tumor features, symptoms, and the treatment plan set by a licensed oncology/urology team. In prostate cancer care, medications may be used to:
- Support symptom control (for example, pain management or urinary symptom support when appropriate)
- Target cancer growth in certain situations (for example, hormone-related approaches and additional systemic medicines in advanced disease)
Do not start, stop, or change medications without clinician guidance.
Treatments
Treatment options and follow-up
Treatment depends on stage, tumor features, and personal priorities. For some people with lower-risk disease, active surveillance (careful monitoring with periodic testing) may be an option instead of immediate treatment. Other approaches can include surgery, radiation, and systemic therapies such as hormone therapy and additional medications for more advanced disease.
Even when prostate cancer is more advanced, treatment can often slow progression and support quality of life—so follow-up care matters.
Prevention and risk reduction
There’s no guaranteed way to prevent prostate cancer, but general risk-reduction steps support overall health:
- Maintain a healthy weight
- Stay physically active
- Eat a balanced diet rich in fruits, vegetables, and whole grains
- Avoid tobacco
If you’re at higher risk, ask a clinician when screening conversations should start.
For a trusted, plain-language overview, see CDC: Should I Get Screened for Prostate Cancer?.
FAQs
Does prostate cancer always cause symptoms?
No. Early prostate cancer often causes no symptoms, which is why it’s sometimes found during screening discussions or testing done for other reasons.
Can urinary symptoms mean prostate cancer?
Sometimes, but many urinary symptoms are caused by non-cancer conditions like benign prostate enlargement or prostatitis. Evaluation matters to find the real cause.
What does “metastatic” prostate cancer mean?
Metastatic disease means the cancer has spread beyond the prostate—often to lymph nodes or bones.
What is active surveillance?
Active surveillance is careful monitoring (with scheduled testing and follow-ups) that may be used for certain lower-risk cases instead of immediate treatment.
Who should consider screening discussions?
CDC notes that men ages 55–69 should make an individual decision after discussing benefits and harms with a clinician, and men 70+ should not be routinely screened.


