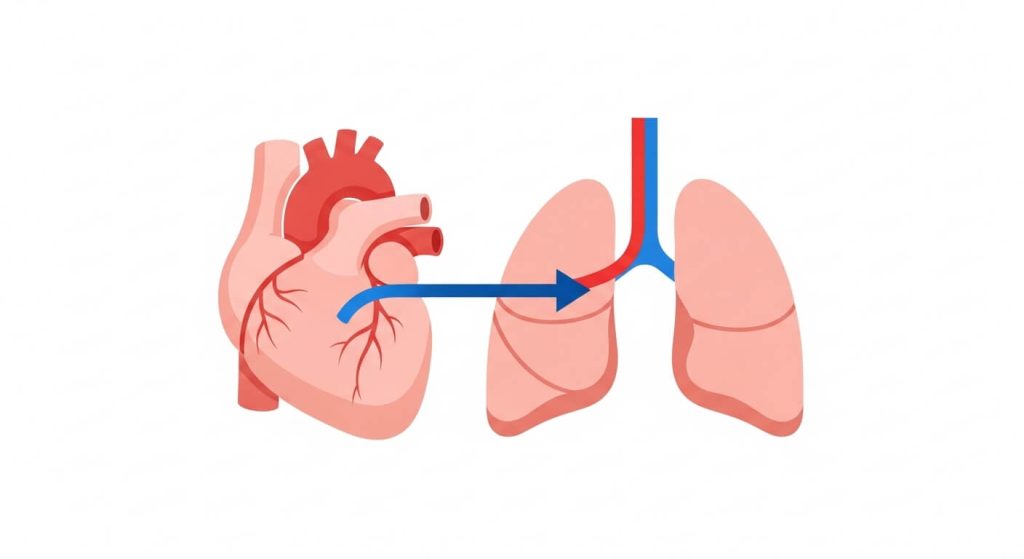
Pulmonary arterial hypertension is a serious form of high blood pressure that affects the arteries in the lungs and the right side of the heart. In this condition, the small lung arteries become narrowed, stiff, blocked, or damaged, so the heart has to push harder to move blood through the lungs.
This page is for education only and does not replace medical care. If you have severe shortness of breath, fainting, chest pain, blue/gray lips, or rapidly worsening symptoms, seek urgent evaluation.
Definition
Pulmonary arterial hypertension (PAH): what it is and why it matters
Pulmonary arterial hypertension (PAH) is a subtype of pulmonary hypertension where the problem begins in the lung arteries themselves (often called “Group 1”). As resistance inside the lung circulation rises, pressure increases and the right ventricle can become strained over time.
Some people live with PAH for years with careful monitoring and treatment. Others progress faster. The goal of care is to reduce pressure and resistance in the lung arteries, protect the right side of the heart, and maintain day-to-day function.
Causes
What causes pulmonary arterial hypertension?
Pulmonary arterial hypertension can develop for different reasons, including:
- Idiopathic PAH: no clear cause is identified.
- Heritable PAH: gene changes in a family can increase risk.
- Drug/toxin exposure: certain appetite suppressants and illicit stimulants have been linked to PAH.
- Associated conditions: connective tissue diseases (such as scleroderma), portal hypertension/cirrhosis, certain congenital heart defects, and some infections can be associated with PAH.
Pulmonary hypertension is also classified into other groups when the main driver is left-heart disease (Group 2), lung disease/low oxygen (Group 3), chronic blood clots in the lung arteries (Group 4), or other mixed/unclear causes (Group 5). Because treatment approaches differ, confirming whether someone has pulmonary arterial hypertension versus another group is a key step.
Symptoms
Symptoms of pulmonary arterial hypertension
Symptoms often develop gradually and may be mistaken for deconditioning or asthma early on. Common symptoms include:
- Shortness of breath (first with activity, sometimes later at rest)
- Fatigue and reduced exercise tolerance
- Chest pressure or chest pain
- Dizziness or fainting (syncope), especially with exertion
- Fast heartbeat or palpitations
- Swelling in the ankles, legs, or abdomen (fluid retention)
Skin or lips that look blue or gray can be a sign of low oxygen. If symptoms are new, worsening, or severe, seek medical evaluation promptly.
Diagnosis
How pulmonary arterial hypertension is diagnosed
Diagnosing pulmonary arterial hypertension usually involves two steps: (1) confirming elevated pressures in the lung circulation, and (2) identifying the most likely cause/group.
Common parts of a workup may include:
- History and exam: symptoms, family history, medication/drug exposures, and signs of right-heart strain.
- Echocardiogram: a noninvasive ultrasound that can estimate pressures and assess right-heart size/function.
- Right heart catheterization: the standard test to confirm PAH and measure pressures directly.
- Blood tests: to look for associated conditions (for example, autoimmune disease markers) and organ strain.
- Pulmonary function tests and oxygen assessment: to evaluate lung disease and oxygen levels.
- Imaging (CT, V/Q scan, or other studies): to assess lung structure and evaluate for chronic clots.
- Exercise testing (6-minute walk test or cardiopulmonary exercise test): to measure functional capacity and response to therapy.
Because pulmonary arterial hypertension is uncommon and management can be specialized, many patients benefit from evaluation at or in coordination with a pulmonary hypertension center.
Medications
Medications used for pulmonary arterial hypertension
Medication choices depend on severity, risk profile, and test results. Common categories used for pulmonary arterial hypertension include:
- Endothelin receptor antagonists (ERAs): help counter vessel narrowing signals.
- PDE-5 inhibitors: help relax lung arteries and improve blood flow.
- Soluble guanylate cyclase stimulators: another pathway to support vessel relaxation (not used with certain other drugs).
- Prostacyclin pathway therapies: inhaled, oral, or infused options that can strongly widen lung vessels and reduce strain.
- Selective calcium channel blockers: used only in a small subset who respond to vasoreactivity testing during catheterization.
- Supportive medicines: diuretics for swelling, oxygen for low levels, and other therapies when clinically indicated.
Never start, stop, or combine prescription therapies for PAH without clinician supervision—some combinations are unsafe or require close monitoring.
Treatments
Treatments and daily steps for pulmonary arterial hypertension
A plan for pulmonary arterial hypertension often combines medications with supportive care and monitoring:
- Regular follow-up: symptom check-ins, labs, imaging, and walking tests to track risk and response.
- Activity planning: many people benefit from supervised rehabilitation or clinician-approved exercise, with pacing and rest.
- Vaccines and infection prevention: respiratory infections can destabilize PAH.
- Salt and fluid guidance: individualized advice may help reduce swelling and right-heart strain.
- Oxygen therapy: if levels are low at rest, with sleep, or during activity.
- Procedures for advanced disease: selected patients may be evaluated for interventions such as atrial septostomy or lung transplantation.
If you already have a clinician-guided plan and valid prescriptions, some people explore affordability options with safety-first planning. Start with our Certified Medical Tourism Professional guide to understand verification and continuity of care.
FAQs
Pulmonary arterial hypertension FAQs
Can PAH be cured?
Pulmonary arterial hypertension is usually a long-term condition. While there isn’t a universal cure, many people can improve symptoms and slow progression with modern therapy, monitoring, and addressing contributing conditions.
Is PAH the same as “regular” high blood pressure?
No. PAH involves elevated pressure in the lung arteries and affects the right side of the heart. Systemic high blood pressure refers to pressure in the body’s main arteries.
Why can PAH cause swelling in the legs or abdomen?
When the right side of the heart is under strain, fluid can build up in the body. Diuretics and tailored salt/fluid strategies may help, but the underlying heart-lung pressures also need treatment.
What symptoms should trigger emergency care?
Call emergency services for severe shortness of breath, fainting, chest pain, coughing up blood, blue/gray lips, or rapidly worsening symptoms—especially if these are new.
What’s the difference between pulmonary arterial hypertension and clot-related pulmonary hypertension?
Pulmonary arterial hypertension is Group 1. Chronic clot-related disease is Group 4 and may involve different testing and treatment options, including procedures to address chronic thromboembolic disease in selected patients.


